Boost Your Productivity and Profits: The Accounting Software You’ve Been Waiting For!
Once upon a time, a group of entrepreneurs found themselves tangled in a web of financial complexities in the bustling kingdom of …

A new study indicates that including social determinants of health in sepsis readmission models could enhance their predictive ability.
In the study, posted this past week in the Journal of American Medical Informatics Association, University of California, San Diego, researchers utilized data from the National Institutes of Health’s All of Us research program cohort.
They found that including different social determinants of health improved the model’s ability to forecast which sepsis patients are at risk of unplanned 30-day readmission.
“Our results highlight the significance of [social determinants of health] in identifying which patients may aid from additional resources around the time of discharge, or post-discharge, to control 30-day readmissions,” wrote the researchers.
WHY IT IS IMPORTANT
As the researchers reported, 30-day readmissions for sepsis – already a prevalent and potentially deadly condition – are more familiar and costly than those for several other states, including acute myocardial infarction, chronic obstructive pulmonary disease, and congestive heart failure.
“Improved systems are required to identify those at the highest risk for readmission, design targeted help for those individuals, and prevent costly readmissions,” they wrote.
“A broader knowledge of contributing factors is therefore indicated, including investigating whether social factors affect readmissions,” they continued.
However, specifying which patients are most at risk is challenging.
Many hospitals use scores not explicitly designed for patients with sepsis to flag those most at risk of readmission.
The UCSD team employed a data set and patient-level survey information from NIH’s All of Us program, including data from 265,833 individuals from 35 hospitals.
“The major finding of this multicenter longitudinal cohort study is that certain [social determinants of health] are deeply associated with unplanned 30-day sepsis readmissions. The inclusion of such information into a predictive model for readmissions can greatly improve predictive ability and model actionability,” the study team stated.
Researchers pinpointed several potentially actionable factors – including poor transportation to receive healthcare, the inability to pay for specific aspects of medical care, and the absence of insurance – strongly associated with 30-day readmission.
Other aspects came into play:
“These have been earlier described as factors for readmission, although not specifically in sepsis patients. It is doubtful if hospital readmission programs are practical when targeting these populations,” read the study.
The research team noted that some elements, such as digital literacy and internet connectivity, were not included in the All Of Us data set, potentially concerning the model’s predictive abilities.
“Nevertheless, the 88 [social determinants of health] variables included in our models greatly improved our predictive performance, highlighting the implication of accounting for such factors in predictive models and the need for further investigation in this domain,” they wrote.
THE BIGGER TREND
Given the expense, frequency, and danger of sepsis, researchers and IT innovators have devoted energy to better predicting the condition in patients. Sometimes, this has peeked like implementing alerts, often powered by artificial intelligence.
However, Dr. Thomas Selva, chief medical information officer at the University of Missouri Healthcare and medical director for the Tiger Institute for Health Innovation, says people’s power is necessary. Selva’s team won a HIMSS Davies Award for its work pairing the National Early Warning Score algorithm with a prompt response team to contribute to a reduction in sepsis mortality.
“All too often in health IT implementations, we put an alert in the system, and it stays there forever, even though it is not accomplishing the goal that you wanted it to achieve,” he stated in an interview with Healthcare IT News this spring.
“You want to make sure there is good evidence behind the alert and then have good reporting measuresg as well,” he said.
Once upon a time, a group of entrepreneurs found themselves tangled in a web of financial complexities in the bustling kingdom of …

A profound revolution is underway in the labyrinth of time, where the threads of innovation and industry intertwine. Modern factories, akin to …
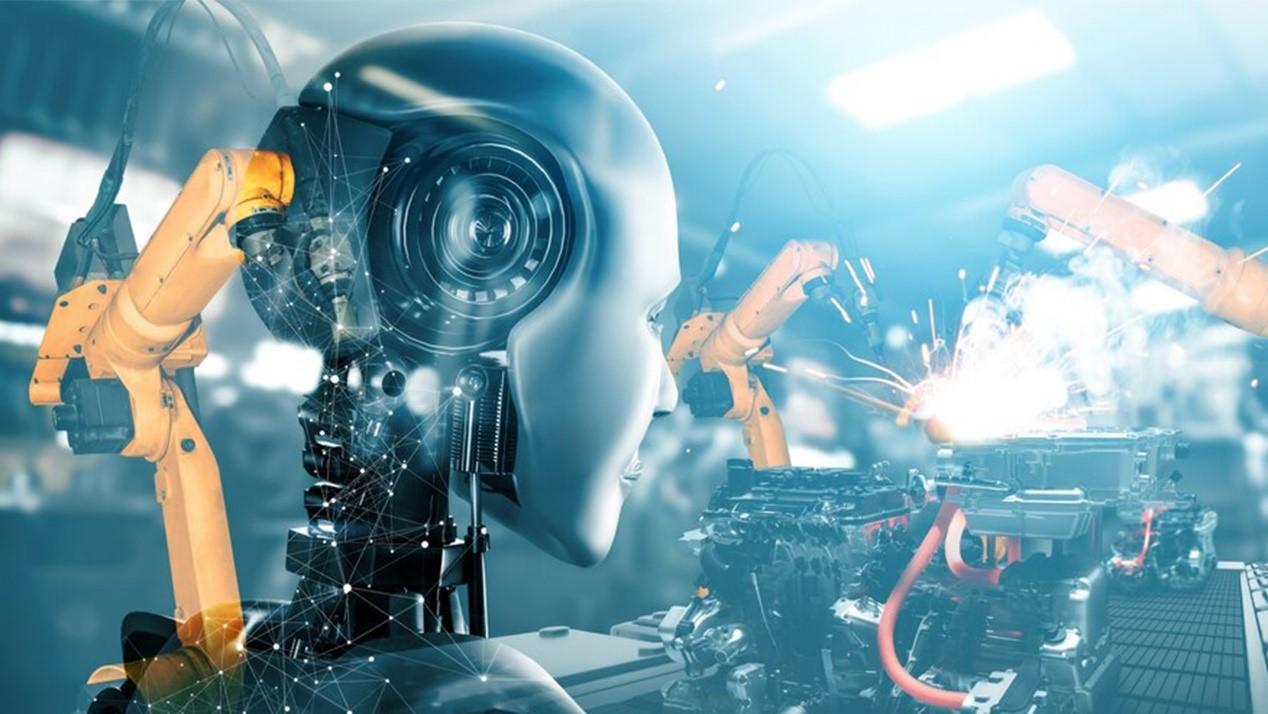
In the annals of human history, the art of manufacturing has undergone a metamorphosis so profound that it has reshaped …

In the labyrinth of modern industry, where the flames of innovation flicker and the winds of change howl, there exist titans—visionaries …